Writing a strong utilization review nurse resume isn’t just about ATS formatting; it’s about knowing what to say, what to leave out, and how to shift the focus from bedside tasks to clinical thinking. And for most nurses making this transition, that’s where things get messy.
If you’re new to considering utilization review roles, learn more about how to become a utilization review nurse and what these positions entail.
Let’s break down the 3 most common resume mistakes nurses make when applying to Utilization Review jobs and what to do instead.
Mistake #1: Listing tasks instead of showing how you think
The first mistake I see most often is assuming the person reading your resume already understands what bedside nurses do. So we end up listing too many clinical tasks like monitoring patients, giving meds, and documenting assessments without explaining what any of it means, how it impacts care, or connecting it to the utilization management nursing job. There’s no context, and no outcomes.
How to fix it:
Start shifting your bullets from task-based to thinking-based. Instead of focusing on what you did, show what you noticed, questioned, or collaborated on.
Did you find something in the documentation that didn’t match the plan of care? Did you help case management clarify discharge readiness? That’s the kind of judgment these roles look for.
It’s totally fine to include some direct care tasks, especially if they’re part of the role’s foundation, but they shouldn’t take up the entire resume. Use them as a base, and then build in examples that show how you thought through what was appropriate, escalated concerns, or helped move care forward.
If your resume is full of words like “administered meds” and “performed assessments,” it’s not speaking the language of the job description that the ATS system or recruiters are looking for. Another tip is to leave off irrelevant bedside certifications unless they are mentioned in the job description.
For guidance on which remote nursing certifications are most valuable for UR roles, check out our certification guide.
Mistake #2: Leaving out measurable impact
The second mistake is not including anything measurable on your utilization review nurse resume. Most of us don’t keep a running list of unit metrics or projects we’ve contributed to, especially if we weren’t leading them, so this part can feel really hard. And honestly, it’s just not something we’re trained to pay attention to in bedside roles.
We show up, take care of our patients, support our team, and move on to the next shift; there’s not always time or space to document what kind of impact we had.
How to fix it:
You don’t need exact numbers for every bullet point, but if you can include even one or two measurable results (5 total for the whole resume is the goal), it can help your resume stand out.
It could be something like a reduction in readmissions, improved discharge times, or patient education that led to better follow-up compliance. You can use unit-level data, too. If your floor reduced falls or improved documentation around restraints, you were part of that outcome, whether you led the project or not.
If you truly don’t have access to metrics, that’s okay. You can still show your impact by describing the change you supported or the outcome your work contributed to by using words that show value, like decreased or increased.. The goal is to move from “I did this task” to “here’s how that task helped move care in the right direction.”
Example:
Original bullet:
Assisted with patient discharges and coordinated follow-up care instructions.
Rewritten (with a metric):
Collaborated with case managers to prepare patients for discharge, contributing to a 15 percent reduction in delays for post-acute referrals.
Rewritten (without a metric):
Worked with case management to coordinate discharge plans and improve documentation accuracy, which helped reduce delays in post-acute referrals.
Mistake #3: Using language that doesn’t match the job
The third mistake is using language that doesn’t match the role. UR hiring managers aren’t just scanning for clinical tasks. They’re looking for signs that you understand medical necessity, documentation standards, and how to think through whether the care being provided matches what’s appropriate for the level of care.
If your resume hasn’t led to interviews yet, it doesn’t mean you’re not qualified. It might just mean it’s not written in a way that lines up with how this type of role views nursing experience.
How to fix it:
Start by reading the job description closely. Look for the exact phrases that show up more than once, things like “InterQual,” “clinical review,” “concurrent review,” or “payers.” Those are keywords for a reason. Once you’ve identified them, go back to your resume and ask: where does your past work touch these areas, even indirectly?
Maybe you’ve collaborated with case management to prep for discharge, or helped clarify admission status during rounds. Even if you’ve never used InterQual, you can mention that you’ve reviewed documentation for discharge readiness or helped escalate level-of-care concerns. The key is to show that you understand how care decisions and documentation are evaluated, not just delivered.
A strong utilization review nurse resume balances clarity with searchability. If it reads beautifully but doesn’t hit ATS keywords, it won’t make it through the initial screening.
I always tell nurses making this transition to think about two skill buckets when it comes to their resume.
One bucket holds the nursing clinical experience you already have. The other needs to be filled with transferable skills that match the role you’re aiming for.
Your resume’s job is to bridge the gap between what you’ve done and what this new role is asking for, so the recruiter or hiring manager can clearly see how your background fits, even if you haven’t worked in UR before.
How to Build a Resume That Speaks to Utilization Review Nurse Hiring Teams
One of the easiest ways to adjust the language on your resume is to pay attention to the keywords that show up in actual Utilization Review job descriptions. These terms help signal that you understand the role, and they also help your resume get picked up by applicant tracking systems (ATS).
Here are some of the most common terms you’ll see across postings from health plans, vendors, and hospital systems:
- InterQual or MCG
- Clinical criteria
- Clinical documentation
- Medical necessity
- ICD-10 and CPT codes
- Admission or discharge planning
- Referral or discharge coordination
- Level-of-care status
- Communication with providers and internal teams
- Collaborates, communicates, consults, evaluates
And here’s where many nurses miss the mark: they don’t take the time to pull keywords from the actual job description. If you want your resume to get past the ATS and in front of a human, you’ll need to reframe your experience using the same language the job is using. Start by looking for ATS keywords (repeated phrases, skills, or tools) in the job description, then use those to adjust your bullet points and professional summary. That small step makes a big difference in how your resume gets read, and whether it moves forward.
You don’t need to force these in, but if you have experience that touches on any of them, or you’ve worked with processes or tools that overlap, those are the terms to use. Even if you haven’t used InterQual or MCG directly, you can mention experience with discharge criteria or reviewing documentation to support transitions in care.
Being able to speak the language of the role is what helps your resume stand out. You probably already have pieces of this experience, you just need to reword it so the connection is clear.
For a ready-to-use framework, check out this ATS-optimized resume template that can help with formatting and structure.
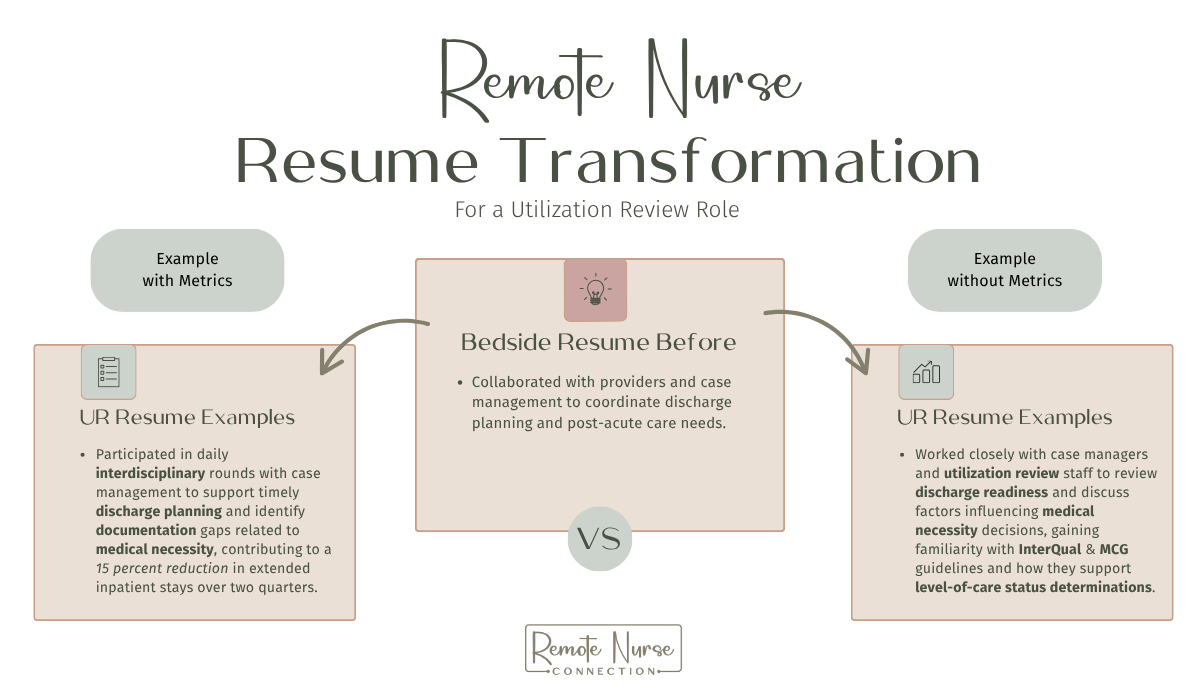
Utilization Review Nurse Resume Example: Before and After Rewrite
By now, you know your resume needs to reflect how you think clinically, not just what you did during your shift. That applies to your work experience bullet points and your professional summary.
Here’s a before-and-after example that shows how a nursing bedside work experience bullet can be reframed to speak more directly to a Utilization Review role.
Example:
Before:
Act as the primary point of contact for families, providing emotional support and clear communication about patient status, procedures, and prognosis.
After (with a metric):
Supported discharge planning for [X] patients/week by coordinating with families and providers, resulting in [Y]% increase in post-discharge follow-up compliance and improved care continuity.
After (without a metric):
Served as a key liaison between the care team and family members, facilitating clear communication around care plans, discharge readiness, and available resources to support safe transitions.
Top ATS Keywords for Utilization Review Nurse Resumes
When applying to UR roles, these are some of the most common terms you’ll want to naturally include in your resume. They come straight from job descriptions across health plans, vendors, and hospital systems:
- Utilization Review
- Medical Necessity
- Concurrent Review
- InterQual or MCG
- CPT / ICD-10 / HCPCS
- Payer Guidelines
- Clinical Documentation
- Appeals & Denials
- Admission Criteria
- Case Management Software (like TruCare, Medecision, GuidingCare)
You don’t need to force these in, but they should show up in ways that match your experience (or state your desire to obtain experience in). Even if you haven’t used InterQual, for example, you can reference working with discharge criteria or clinical decision-making tools if relevant.
Most of the nurses I work with feel stuck not because they don’t have the skills, but because they don’t know how to talk about those skills on their resume in a way that fits this kind of role.
Recap: What Actually Makes a Strong Utilization Review Nurse Resume
If your resume hasn’t led to interviews, it’s probably not because you’re missing the skills. It’s because the way you’re presenting those skills doesn’t line up with what UR/UM hiring managers are actually looking for.
By now, you know the common mistakes to avoid:
Listing tasks without showing how you think
Leaving out measurable results or impact
Using bedside language instead of UR language
And you’ve seen how to fix them:
Shift your bullets to show decision-making, not just duties
Use unit-level data or describe the impact you contributed to
Pull ATS keywords from the job description and rework your phrasing to match
You don’t need to start from scratch or add random words to your resume to get past the ATS scan. You just need to reframe what you already know and do every day as a nurse through the lens of documentation, level of care appropriateness, and clinical judgment.
For additional resume writing tips that apply across all nursing roles, our comprehensive post covers the fundamentals.
That’s what makes a resume stand out for a Utilization Review role.
FAQ’s
What can I do to make my resume stand out?
Most nurses don’t realize that getting certified in MCG guidelines can significantly boost their resume. Usually, employers sponsor this certification, creating that “catch 22” scenario of can’t get hired without experience, but there’s another way to get it.
The Case Management Institute (CMI) partnered with MCG Health, which gives you eligibility to take the certification exam on your own after successfully passing their course. This is a great move if you’re looking to break into UR nursing without employer sponsorship.
👉 Check out the Utilization Management & MCG course at CMI (use code ‘andrea10’ for 10% off)
For more context on the difference between Utilization Review and Utilization Management, check out CMI’s post: Nursing Beyond the Bedside
How do I show Utilization Review related experience if I’ve only worked bedside?
This is one of the most common questions I get and the answer is: it’s all about how you frame your experience.
If you’ve ever participated in discharge planning discussions, found documentation issues, or worked closely with case managers to determine next steps for a patient, you’re already working with skills that transfer directly into UR. You can write bullets like:
“Collaborated with case management to assess discharge readiness and remove barriers to timely transitions, improving alignment with level-of-care criteria and payer expectations.”
Or:
“Reviewed provider documentation and escalated concerns related to treatment appropriateness, which helped reduce discharge delays and improve documentation quality.”
You’re not claiming to have done formal utilization review; you’re showing that you’ve been part of the process and understand how it works. That honesty, paired with the right language, is what helps get your foot in the door.
What is considered utilization review experience?
Utilization Review experience doesn’t have to mean you’ve already worked in a UR role. Employers often consider related experience like:
- Participating in interdisciplinary rounds or discharge planning
- Collaborating with case managers or UR nurses
- Reviewing documentation for accuracy, consistency, or completeness
- Escalating concerns when treatment didn’t match clinical expectations
- Understanding payer criteria or admission status (even if you weren’t the decision-maker)
If you’ve done these things, even informally, you can include them on your resume. It’s about showing that you already think like a reviewer, even if your title didn’t say “UR Nurse.”
Do Utilization Review nurses talk to patients?
In most UR roles, especially remote ones, nurses are reviewing records, not calling or assessing patients directly. That said, there are exceptions.
Generally speaking, these roles are more about evaluating documentation, applying clinical criteria like InterQual or MCG, and communicating with internal teams, providers, or insurance reps, not patient-facing care.
What are the goals of a Utilization Review nurse?
The main goal of a UR nurse is to make sure patients are receiving the right care, at the right time, in the right setting, and that it’s supported by clinical documentation. You’re essentially looking at whether the care being provided meets medical necessity criteria based on payer guidelines.
That can include:
- Reviewing hospital admissions for appropriateness
- Determining if continued stays are justified
- Preventing unnecessary procedures or extended inpatient days
- Ensuring the documentation supports the level of care billed
Think of it as applying your clinical judgment through the lens of quality, policy, and reimbursement, not just patient care.
Ready to Stop Guessing What to Put on Your Utilization Review Nurse Resume?
Figuring out how to shift your bedside experience into something that fits Utilization Review can be tough, especially if you’ve never seen what that’s supposed to look like.
You don’t have to guess your way through this. Once you see how other nurses are framing their experience, using the exact language hiring teams are looking for, it starts to click.
Inside the Premium Membership, you’ll get access to real resume examples based on actual Utilization Review/Management job descriptions, guidance on what hiring managers are really looking for, and examples to help you rewrite your resume in a way that actually fits the role.
Remote Nurse Connection is proudly Ad-free. All opinions are my own. This post may contain affiliate links, which means I’ll receive a commission if you purchase through my link, at no extra cost to you. As an Amazon Associate, I earn from qualifying purchases. Please read full disclosure here.
Browse A Bit More On the Blog…
Want a Less Stressful Nursing Job? Here’s How to Become a Nurse Data Abstractor
Jun 17, 2025
If you’ve been searching for a less stressful, flexible remote nursing job that lets you work from home and still use your clinical knowledge, you’ve probably come across roles like “nurse data abstractor.” But trying to figure out what the job actually involves or,...
CDI Nurse Career Guide: How to Become a Clinical Documentation Improvement Specialist
Jun 2, 2025
Clinical Documentation Improvement (CDI) nurses do just that: improve documentation. The goal is to clarify and improve the medical record so there aren't any gaps or missing notes that may prevent accurate billing and reimbursement, and so the complete clinical...

Your Insider Connection to Remote Nursing Success
I help nurses find the best-fit remote jobs that bring flexibility, personal freedom and alignment, and continued professional growth.
CATEGORIES
Free Getting Started Guide
FOR LANDING A
REMOTE NURSING POSITION!